Now at the moment, the press is very much focused on the death rate, and rightly so. We are taking either the illness seriously or not seriously based on the death rate in our local area or our country. Based on that, we're deciding what our level of danger is. But in fact, something that's being missed is that there's a lots of reports of people suffering from post-viral fatigue syndromes as a result of having the COVID-19 illness. This isn't surprising...
Let me just share with you some of the things that we've been researching and finding. We found that yes, there is some evidence that many people who perhaps survive the condition, perhaps to have it moderately or even severely, they survive it, but in fact, for many months, and obviously it's only been a couple of months since the first, what, two or three months since the main wave happened, that they still experience symptoms ongoing. A world-leading infectious disease expert, the editor of the Cochrane Report, Professor Paul Ghana, he actually suffered from the illness himself. He had COVID-19 and he actually said, "Every day there has been extreme emotions, extreme fatigue. There's been something new each day, a muggy head, upset stomach, tinnitus, pins and needles, aching all over, breathlessness or dizziness." Some other reports show that even people with mild illness have experienced some longer-lasting symptoms. People have reported that a small percentage of people who perhaps were infected in February or March are still experiencing some fatigue, headaches, breathlessness, and problems concentrating, or doing even light exercise.

For those people who suffer from any and chronic fatigue syndrome, you'll certainly recognize some of those symptoms. In Italy, a director of the San Mateo Hospital in Pavia says some of the longest-suffering Italians are finding themselves in physical and financial uncertainty, unable to shake sickness and fatigue and get back to work. We've seen many cases in which people take a long, long time to recover. It's not the sickness that is lasting for 60 days. It's the convalescence or the period of recovery. It's a very long period.
I need to highlight today that it's not just the risk or danger passing away from this condition, but it's also the effects that it can have on us as individuals. What I'd like to share with you is actually our model for how we look at why some of these illnesses turn into longer-term issues and share that with you so that if there are medical practitioners, doctors, or people who are suffering from the condition around you, you have some information that you can share with them.
Now, what exactly is this corona virus? What is COVID-19? Well, it's a novel virus. It was only recognized late last year. And first of all, it infects generally the nose. And if our epithelial cells, our immune cells in our nose and the back of the nose are able to defend against the virus, then it can be fought off then and there. Then it travels down the back of our nasal cavity into our throat area.
And once again, we have our immune system to fight it off at that location. And if our immune system isn't strong enough and we don't manage to fight it off, it then continues into our lungs, and that's when people experience more severe illness. At that point in time, it's very interesting. People think that we're dying from the actual virus itself, but in fact, it's our own immune system response to the virus which is making many patients pass away. And it is because of the pneumonia.
So what happens is, our immune system over responds to the virus. Now, why would that be? Within our model, our whole body, our whole nervous system, our whole brain, everything about it is designed for survival, survival of our genes. Passing them on to the next generation. And so, when our bodies and our brains experience a threat, the number one priority is to defend against that virus and ensure survival, or that pathogen.
So when it starts invading the lungs, the immune system goes into this hyper response. It believes that, "Because I haven't been able to fight off this virus as it's transported down this respiratory tract, it's becoming more and more serious. Therefore, I need to unleash the best possible immune response that I can. I need to garner all the forces that I can to defend against it, because my priority is ensuring survival."
And that's why we get something known as a cytokine storm, where these chemical messages start informing the entire of the immune system to start fighting against the virus. But of course, when our bodies do that, it causes excess inflammation in our lungs, and also around the body. So there's evidence of inflammation in the brain, there's evidence of inflammation in the liver, and also the kidneys.
And as a result of that, that's where we then get severe inflammation of the lungs, pneumonia, and then the body finds it difficult to breathe. And this is especially so in certain types of patients that perhaps have a weak immune system. We also know that those people who are obese have a higher chance of complications occurring, and those who smoke. So similar risk factors to general disease.

And at that point in time, that's when the person's life is in danger, when we've got that cytokine storm and there's excess inflammation. Now, let's say someone recovers from that. There are two types of illness which may then still occur afterwards. So the first illness may well be weakness in the lungs, and in certain parts of the body, as a result of the inflammation that occurs.
So we call it acute respiratory distress syndrome. That's when this cytokine storm occurs and we get inflammation of the lungs, and then potentially death. Now, at that point in time, those particular responses may have caused some scarring in the lungs, or scarring other parts of the body, which can then cause ongoing debilitating symptoms for people. Now that's not what we're talking about here. That is something that happens also as a result of other illnesses.
What we're talking about are the more moderate cases where actually, there isn't necessarily any scarring in the lungs or any scarring in other parts of the body, but people are still experiencing what we call post-viral fatigue syndrome. Now, post-viral fatigue syndrome is when there's still a general weakness in the system. And why would that be? And it's still a mystery to researchers and doctors.
And here at the Gupta program, we have a model of what might be occurring. Essentially, when the brain goes into that hyper defense mode or hyper response mode, it has over triggered the immune system and also the nervous system. We also experience severe emotions, and emotions are kind of protective stimuli to warn us against danger. Even once the condition is gone, even once the ARDS has gone, the COVID-19 has been fought off, the system may still be primed in that alert mode.
It still may be primed to watch out, because if you've just been through a traumatic experience, just like war veterans experienced trauma in battles or in foreign countries, when they come back, even though the war is over, that particular war veteran, that soldier can still experience severe panic attacks or anxiety. It's because the body still believes that we're in danger.
And analogously to that, If there is trauma as an experience of going through COVID-19, the nervous system and the immune system stay in a traumatized state, a conditioned state. And therefore any mild triggers, for instance, opportunistic infections in the body, perhaps some anxious experiences. Perhaps the symptoms themselves of an overstimulated immune system, they become triggers for our own immune system to keep responding.
So that means that even once the battle is over, the war has been won, our soldiers are still battling. Our immune system is still defending against that pathogen, just in case. The immune system always errs on the side of caution and says, "My priority is survival. And if it means that I've got to be primed and ready to defend against the next wave of attackers, that's what I'm going to do." Because our immune system doesn't care about whether we feel healthy and strong, our immune system cares about survival. That is its number one priority.
And that may well explain why there are many patients who seem to be going on to develop post-viral syndromes. And those post-viral syndromes aren't formally diagnosed as chronic fatigue syndrome or ME until it's been at least six months of that experience, because we know many people experience post-viral fatigue as a result of many different illnesses, including flu.

And so, I'd like to offer that explanation so that it gives us a background and an understanding for it medical researchers, medical practitioners, but also for the general public. That this may be a mechanism by which there are those experiences of post-viral fatigue syndrome. Now, most importantly, what can we do about that? Why is the brain stuck in that loop?
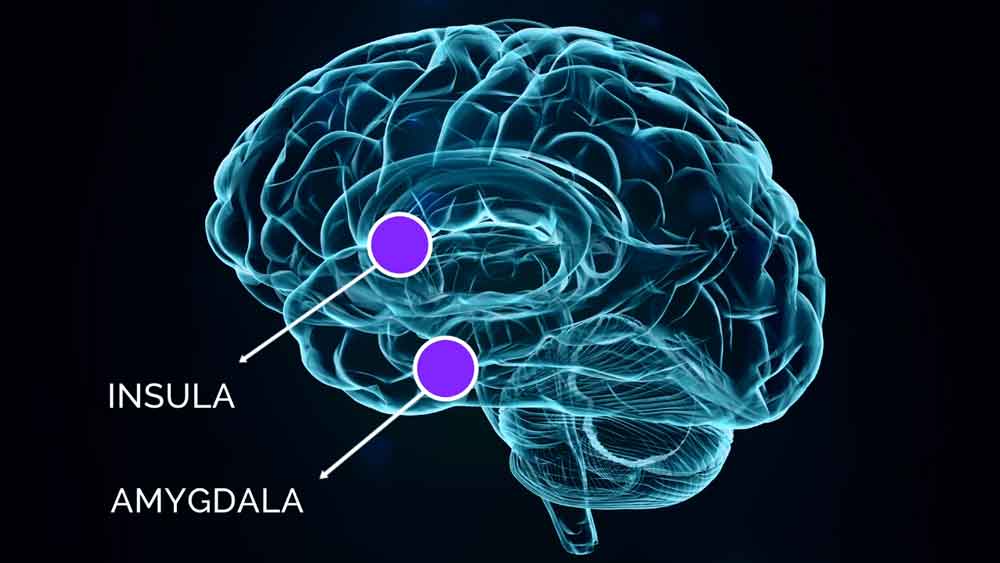
Well, for those of you who know and follow the Gupta Program, we mention two brain structures specifically, the amygdala and the insula. Now, the amygdala's job is to protect us from physical dangers, but also it is involved in immune dangers. And the insula's job is to process the incoming stimuli from the body, see what the appropriate response is, whether that's an immune response or a physiological response. And then enact the correct response to ensure survival.
And the insula is also involved in pain responses, for moderating pain responses. So it's almost like a sentinel that keeps a watch over the body and what's going on, and then protects us from dangers using the appropriate responses. Now we know from animal studies, they find that if you give rats and immunosuppressant combined with sugary water, their immune systems are suppressed.
Now, after a few rounds of doing that, they can give rats just the sweet water without the immunosuppressant, and their immune systems still suppress themselves. The reason that is, is because the immune system will defend against anything which reminds it of the original events, the original illness. So that's why we know that these conditioning events occur in the amygdala and the insula. And that's been proven in animal studies.
In order for those conditioning responses not to occur, what's incredibly important is if you yourself experienced COVID-19, or someone around you experiences that kind of illness, the number one priority is boosting your immune system and taking rest. We live in a very macho culture right now, where when someone experiences illness, we're taught, "Oh, it's man flu. Let's just dismiss it. It's man flu. They're just away from the office because they think they're ill."
And I really want us to take this illness seriously, because of what we're seeing in the research. It clearly has a profound effect on the brain and the body. It clearly is offering certain post-viral syndromes in many patients. And therefore if we do contract it, it is important that we do whatever we can to boost our immune system. Now, number one priority is not rushing back to work.

So if you know people who've had it or who are experiencing certain relapses of what they think is the COVID-19, please do give them the advice to take as much rest as possible, and only to go back to work once they feel ready to do so. That's the number one priority, is to take your time to get back to work if you've experienced it, or someone you know has experienced it.
And secondly, we know that there are certain things you can do to lower that immune over response, or to modulate or moderate that response. Number one are things like meditation. So we know that whether you want to call it meditation or deep relaxation exercises, anything that really triggers your parasympathetic nervous system has the ability to calm that overactive immune response.
So we know that meditation switches off about 30 or 40 genes that are involved in those immune responses. So something like that can really, really help someone recover much better. And of course, there are changes to your diet that you can make as well. And we'll talk about that a bit later. And for those of us who have experienced any chronic fatigue syndrome, it's also important not to exercise. You can't exercise your way out of post-viral fatigue syndrome.
And that's why people who have experienced it, and who perhaps don't know what to do, are often trying to go to the gym or exercise to try and feel better, but that will only make things worse, because it will tell your amygdala and your insula, those parts of the brain, that you're still in danger. And therefore, why are you exercising? You need to rest. So our immune system also gives us triggers to make sure that we rest as well.
And really, it's about making sure that if we're experiencing this post-viral fatigue syndrome, even as a result of flu, or as I said, as a result of COVID-19, we do whatever we can to deeply rest. Even if it's bedrest, even if it's meditating regularly and deeply. All of these things can support the rebalancing of our immune system and bring us back to that stillness.
And if we don't, what then happen, and this is what we're trying to prevent here at the clinic, there could be another wave of ME, chronic fatigue syndrome and fibromyalgia. From patients that in those first few months, after having the condition, especially those few weeks after having the COVID-19, they're not resting. They're not deeply rejuvenating their mind and body.
And that's why we think this is such important information to get out there, so please do share this with your family and friends. And if you're on Facebook or you're joining us on Instagram, please do share this particular video on your newsfeed. You can just click under the video, click the share, and share it on your timeline. Perhaps might share it on support groups or advocacy groups for COVID-19, or other chronic illnesses.
And let's get this information out there, because it could be life saving information. and it can help prevent chronic illness from occurring in people around us.
For more information please watch my video here or click the image below.

Ashok
Ashok Gupta is the Director of the Gupta Program. He has dedicated his life to helping people get their life back from Chronic Illness, improving people’s well-being, and helping them achieve their potential. He has been teaching meditation around the world for over 15 years. He runs a global e-clinic specializing in treating ME, Chronic Fatigue Syndrome, Fibromyalgia & Multiple Chemical Sensitivities – guptaprogram.com
Ashok has spent many years researching the brain neurology of emotion and linking well-being tools with science. He has published medical papers on the basis of stress-related illnesses. He has appeared in many media as an expert on stress on the BBC, CNN, Guardian Newspaper, ITV, The Independent, and many others.
He wrote and presented the Meaning of Life Experiment which is a Free, Award-winning Meditation and Self-Development App www.themeaningoflife.tv
He also works with companies around the world, teaching courses in Leadership, Time Management, and Personal Development. www.ashokgupta.tv